Income Equality – Limited Access to Quality Education
September 4, 2024
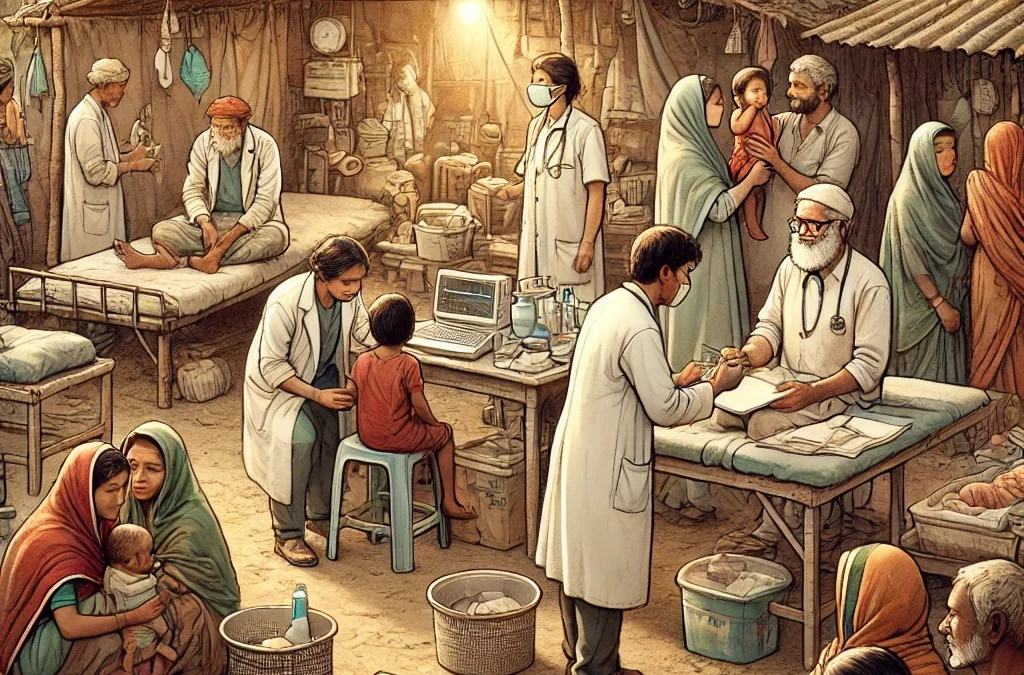
Improving Access to Healthcare – How can Collective Approach help?
September 6, 2024As of today, only about 30-40% of the population in India has consistent and regular access to quality healthcare services if we consider both availability and affordability. This figure highlights the challenges India faces in ensuring equitable healthcare access across its diverse populations.
What are the reasons for lack of access to healthcare, particularly in the underprivileged population in India both in urban and rural areas?
The underprivileged population depends on facilities provided by the government to access healthcare. These facilities are Primary health centers, community health centers, and district hospitals.
According to a National Health Mission report, around 60-70% of the population has access to a primary health center within a 5 km radius. Around 30 to 40% of the population lacks access to primary health care due to the inadequate number of PHCs for the size of the population. Poor transportation and connectivity in rural areas makes it difficult for poor people to reach healthcare facilities, especially in emergencies.
For the remaining 60 to 70%, there are glaring problems that impart the qualitative delivery of healthcare such as
Inadequate Primary Healthcare Infrastructure
Inadequate Buildings: Many PHCs operate out of dilapidated buildings and lack essential amenities like clean water, electricity, and proper sanitation facilities.
Insufficient Space: PHCs often lack sufficient space for examination rooms, pharmacies, and waiting areas, which affects patient privacy and overall service delivery.
Inadequate Medical Equipment: Many PHCs lack basic medical equipment such as X-ray machines, diagnostic tools, and essential items like beds, stretchers, and surgical instruments.
Shortage of Healthcare Personnel:
Doctor-to-Patient Ratio: The World Health Organization recommends a doctor-to-patient ratio of 1:1000. In India, the ratio is closer to 1:1500, with significant disparities between urban and rural areas.
Vacancies and Understaffing at Health Facilities: There is a significant shortage of doctors, nurses, and other healthcare professionals, especially in rural PHCs. The doctor-to-patient ratio in many regions is far below the recommended levels. Apart from doctors, there is a severe shortage of nurses and ANMs. There are qualified personnel available to work in hospitals but there is a lag in filling these vacancies for several reasons. Another issue that ails healthcare is understaffing. The number of personnel working is far less than required to effectively cover the population in these areas.
Absenteeism: High rate of absenteeism among rural healthcare staff leaves many PHCs unable to provide qualitative healthcare.
Lack of Essential Medicines and Supplies
Stockouts and Shortages: Many PHCs frequently experience stockouts of essential medicines, vaccines, and medical supplies, forcing patients to purchase these from private pharmacies, which can be a financial burden on the patient. Poor management of inventory with a lack of technology to update stock plays a crucial role in this problem. Apart from the lack of software to enter the details of stock dispensed there is a lack of computers in the location to update the stock on regular basis.
This also leads to another problem of lack of intelligence to understand what the critical medicines required in the area.
Poor Supply Chain Management: Inefficient supply chain management leads to delays in the procurement and distribution of medicines and supplies, further impacting service delivery.
Inadequate Technology and Digital Infrastructure
Lack of IT Infrastructure: Some PHCs lack computers, internet connectivity, and other IT infrastructure necessary for maintaining electronic health records, records of medicines dispersed, diagnostics conducted, etc. which has an impact on the supply side for both medicines and diagnostics and lack of health records of the patient for effective follow-up.
Limited Telemedicine Capabilities: Telemedicine cannot thrive until we have all the diagnostics present in PHCs which are sadly lacking as of today. What can effectively bridge the gap in healthcare access is underutilized due to the lack of both technological and physical infrastructure in many PHCs.
Limited Laboratory and Diagnostic Services
Lack of Laboratories: Many PHCs lack basic laboratory facilities to conduct routine tests such as blood tests, urine tests, and other diagnostic services. Patients are referred to distant facilities for these tests or to private diagnostic services which defeats the purpose of free healthcare.
Poor Diagnostic Equipment: Even when laboratories exist, they may lack essential diagnostic equipment or face issues like frequent breakdowns and lack of maintenance.
Out-of-Pocket Expenditure:
India has one of the highest out-of-pocket expenditures on healthcare in the world, with over 60% of healthcare costs paid directly by patients. This financial barrier limits regular access to healthcare for a sizable portion of the population despite having insurance schemes.
Inadequate Referral Systems
Poor Connectivity to Higher-Level Care: Many PHCs have weak referral systems with patients referred to higher facilities like Community Health Centers and District hospitals without the names of doctors or specializations that will be treating them. Inadequate coordination and communication between healthcare facilities like Community Health Centers (CHCs) and District Hospitals results in a lack of confidence in patients to visit higher-level healthcare units.
Transportation Issues: The lack of ambulances, lack of fuel, and drivers, and other transportation options makes it difficult for PHCs to refer patients to higher-level care facilities in case of emergencies.
Health Insurance Coverage:
In India, about 35 to 40% of the population is covered under some form of health insurance, either public or private. Ayushman Bharat – PM-JAY alone covers around five hundred million people (50 crore people), making it the world’s largest government-funded health insurance scheme. Despite high coverage, the implementation and accessibility remain challenging in some regions.
Lack of Continuous Medical Education and Training
Limited Training Opportunities: Healthcare staff at PHCs often have limited opportunities for continuous medical education and training, leading to gaps in knowledge and skills, particularly in handling complex cases or emergencies.
Outdated Practices: Without regular training and adequate infrastructure healthcare providers rely on outdated practices which hurt the quality of care.
Inadequate Health Awareness and Outreach
Limited Preventive Services: PHCs often struggle to provide adequate preventive healthcare services, such as immunization, maternal and child health services, and health education, due to resource constraints.
Lack of Outreach Programs: There is often a lack of effective outreach programs to educate the community about health issues and encourage the use of PHC services.
We at Sheya Foundation are passionate about creating a more equitable healthcare system in India.
It is critical to address challenges in healthcare infrastructure to ensure healthcare services reach underserved populations effectively.
In this writeup, we explore what are the gaps in healthcare access so that we can work on doable solutions!